INTRODUCTION TO CERVICAL CANCER
INTRODUCTION TO CERVICAL CANCER
Cervical Cancer: What Every Woman Should Know — And Why Prevention Matters

Cervical cancer is one of the few cancers that can be prevented, detected early, and successfully treated—yet it continues to claim the lives of hundreds of thousands of women every year. With the right information, access to care, and timely action, this disease does not have to be a death sentence.
The Big Picture: Why Cervical Cancer Deserves Attention
Cervical cancer is currently the fourth most common cancer affecting women worldwide. In 2022 alone, an estimated 660,000 women were newly diagnosed, and about 350,000 lives were lost. Tragically, nearly 94% of these deaths occurred in low- and middle-income countries, where access to HPV vaccination, regular screening, and timely treatment remains limited.
Regions such as sub-Saharan Africa, Central America, and South-East Asia carry the heaviest burden. These disparities are driven not only by gaps in healthcare services but also by broader social challenges such as poverty, gender inequality, and limited health education.
The Link Between HPV, HIV, and Cervical Cancer
Almost all cases of cervical cancer are caused by persistent infection with the human papillomavirus (HPV)—a very common sexually transmitted virus. Most sexually active people will encounter HPV at some point in their lives, often without any symptoms. In many cases, the body clears the virus naturally. However, when certain high-risk HPV types persist, they can cause abnormal cell changes that may develop into cancer over time.
Women living with HIV face a much higher risk. They are six times more likely to develop cervical cancer than women without HIV, and about 5% of cervical cancer cases globally are linked to HIV. Because cervical cancer often affects women at a younger age, its impact goes beyond health—one in five children who lose a mother to cancer lose her due to cervical cancer.
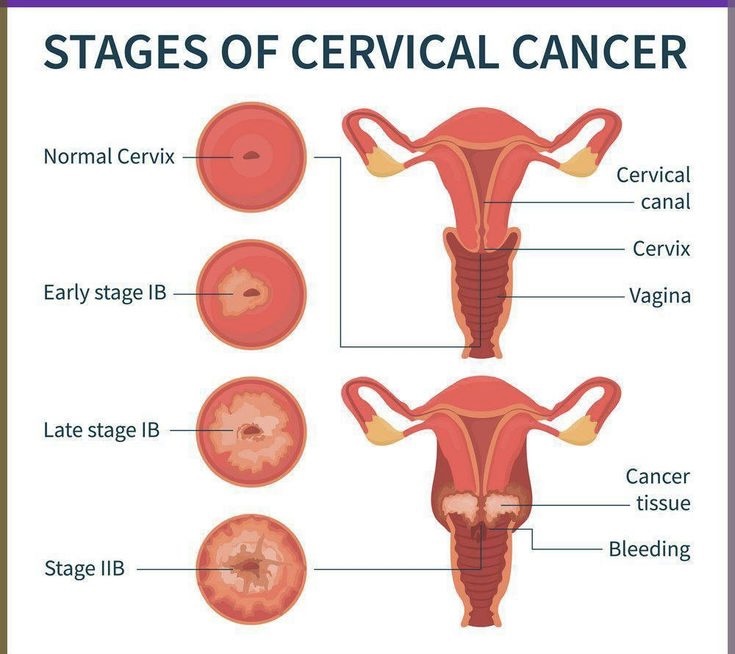
How Cervical Cancer Develops
Persistent infection with high-risk HPV types—especially HPV 16 and 18—can lead to precancerous changes in the cervix, the lower part of the uterus that opens into the vagina. If left untreated, these changes are responsible for about 95% of cervical cancer cases.
In most women, it takes 15–20 years for these abnormal cells to turn into cancer. For women with weakened immune systems, such as those with untreated HIV, this process can happen much faster—sometimes within 5–10 years. Other factors that increase the risk include smoking, having multiple births, early pregnancy, long-term hormonal contraceptive use, and co-existing sexually transmitted infections.
Prevention Starts With Knowledge and Access
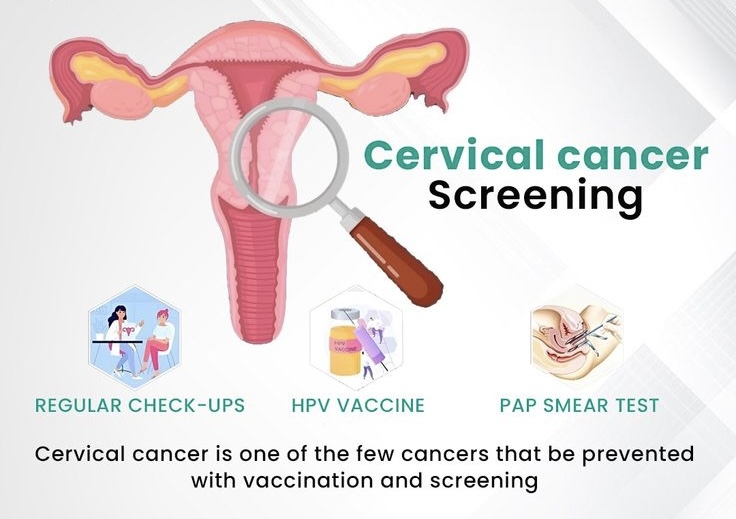
Cervical cancer prevention is possible at every stage of life. Key strategies include:
• HPV vaccination for girls aged 9–14 years, which is highly effective in preventing HPV infection and related cancers
• Regular cervical screening, starting from age 30 (or 25 for women living with HIV), to detect precancerous changes early
• Prompt treatment for women who show symptoms or test positive during screening
When cervical cancer is detected early and treated properly, it can be cured.
HPV Vaccination: A Powerful First Line of Defense
As of 2025, eight HPV vaccines are licensed globally, with five approved by the World Health Organization (WHO). All of them protect against HPV types 16 and 18, which cause about 76% of cervical cancers.
Most countries recommend one or two doses for girls aged 9–14. People with weakened immune systems, including those living with HIV, may need two or three doses. Some countries also vaccinate boys to reduce HPV spread and protect men from HPV-related cancers.
Additional ways to lower the risk of HPV infection include:
• Avoiding or quitting smoking
• Using condoms
• Voluntary male circumcision
Screening and Treating Precancer Saves Lives
Cervical screening is essential because precancerous changes usually cause no symptoms. Even vaccinated women still need regular screening.
Women are advised to:
• Get screened every 5–10 years starting at age 30
• Screen every 3–5 years starting at age 25 if living with HIV
WHO recommends at least two lifetime screenings—by ages 35 and 45.
Self-collection of samples for HPV testing is now available in many settings and has proven to be just as reliable as samples collected by healthcare providers, making screening more accessible and comfortable.
When precancer is detected, treatment is simple, quick, and highly effective. It may involve techniques such as thermal ablation, cryotherapy, LEEP/LEETZ, or cone biopsy—often with minimal discomfort.
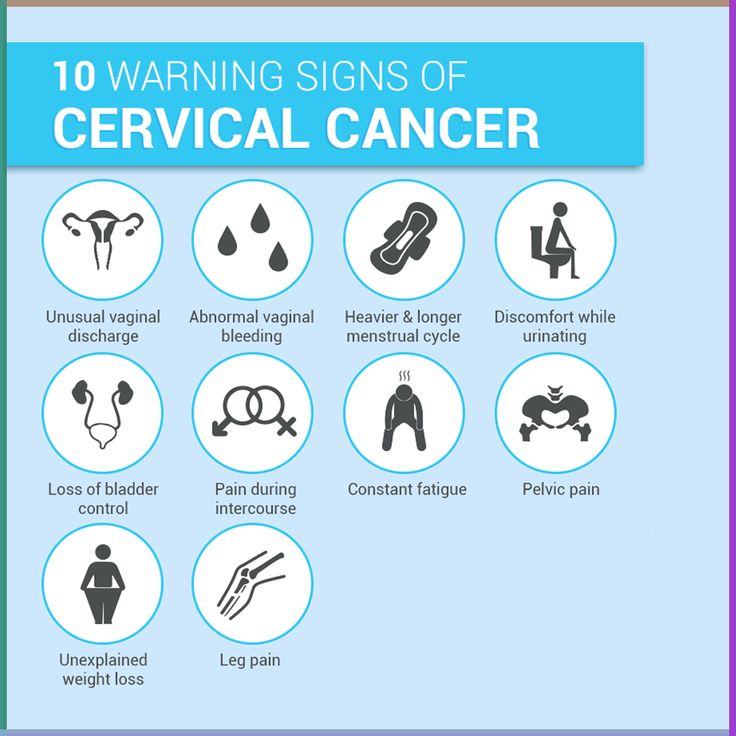
Recognizing Symptoms and Seeking Care Early
Early-stage cervical cancer is highly treatable. Women should seek medical attention if they experience:
• Unusual bleeding (between periods, after sex, or after menopause)
• Persistent or foul-smelling vaginal discharge
• Ongoing pelvic, back, or leg pain
• Unexplained weight loss, fatigue, or loss of appetite
• Vaginal discomfort or leg swelling
Diagnosis may involve imaging, biopsy, and laboratory testing, followed by appropriate treatment such as surgery, radiotherapy, chemotherapy, and supportive care.
A Global Commitment to Elimination
Every country has committed to eliminating cervical cancer as a public health problem. The WHO Global Strategy aims to reduce new cases to fewer than 4 per 100,000 women by achieving the 90–70–90 targets by 2030:
• 90% of girls fully vaccinated with HPV vaccine by age 15
• 70% of women screened by ages 35 and 45
• 90% of women with cervical disease receiving treatment
Experts estimate that meeting these goals could prevent 74 million new cases and save 62 million lives by 2120.
World Cervical Cancer Elimination Day
Every year on 17 November, the world marks World Cervical Cancer Elimination Day—a moment to raise awareness, support women and girls, and strengthen collective action toward prevention, screening, and treatment.
At Eagle Eye Foundation, we believe that no woman should die from a preventable disease. Awareness, early action, and equitable access to healthcare can change the story of cervical cancer—for individuals, families, and entire communities.
Comments
No comments yet.